9 Exceptional Decades of Raw Milk Licensing in NY State?
I was surprised to find a reference to the year 1924 as the first year that NY State licensed a raw milk dairy. While I requested the CDC NORS dataset on outbreaks and illnesses beginning in 2005 and not 1924, the record of safety in NY state in recent decades is outstanding.
In the previous 10 years, only 4 illnesses from one outbreak were attributed to raw milk in NY state. For 2005-2022, a total of 58 illnesses (4 hospitalizations, no deaths) were attributed to NY State raw milk. CDC reports that all 58 illnesses were associated with campylobacteriosis.
No outbreaks were reported for 4 other pathogens that NY State includes in periodic testing: Listeria monocytogenes; pathogenic E. coli (STEC/EHEC/VTEC/O157:H7); Salmonella; and Staphylococcus aureus (Stephenson et al., 2024).
Although numbers of NY State licences have increased in recent years, no increasing trend in the burden of illness was observed for raw milk. Neither is the rate of illnesses associated with raw milk in any state increasing (Coleman and North, 2023; Stephenson et al., 2024). The figure below lists CDC NORS outbreaks from 2005-2022 associated with raw milk in NY state in orange symbols for the right axis (0, 1, 2, or 3 outbreaks per year) and numbers of NY State licenses for the left axis (10 to 82 licenses per year). The rate of illness adjusted for US Census data for NY State was less than 1 illness in 6 million person-years (Stephenson et al., 2024). Between 2 and 20 people became ill in each NY State outbreak associated with raw milk since 2005.
Although data on raw milk production in NY state is not compiled, evidence exists that demand for raw milk is increasing, despite warnings consistent with the ‘risk perception’ that ‘raw milk is inherently dangerous’. Note that the figure below on California retail raw milk sales is Supplemental FIgure 1 in the first Risk Analysis manuscript on influenza H5N1 (Coleman, 2025).
Risk Analysts defined ‘risk perception’ as follows: ‘a person’s subjective judgement or appraisal of risk’ (Society for Risk Analysis Glossary, 2018); and ‘a blending of science and judgement with important psychological, social, cultural, and political factors’ (Slovic, 1999). Thus, ‘risk perceptions’ are social constructs reflecting ideology, beliefs, and economic interests; ‘risk perceptions’ are not estimations based on the accepted framework for evaluating and incorporating scientific evidence (Marks et al., 1998; Codex Alimentarius Commission, 1999) and quality analysis (Jones and Adida, 2011; Waller et al., 2024; Lathrop et al., 2024) for robust risk analysis. Neither was the work of Chen et al. (2025) based on the established framework for assessing transmission of influenza (Kingley and Nguyen-Van-Tam, 2013; Coleman, 2025).
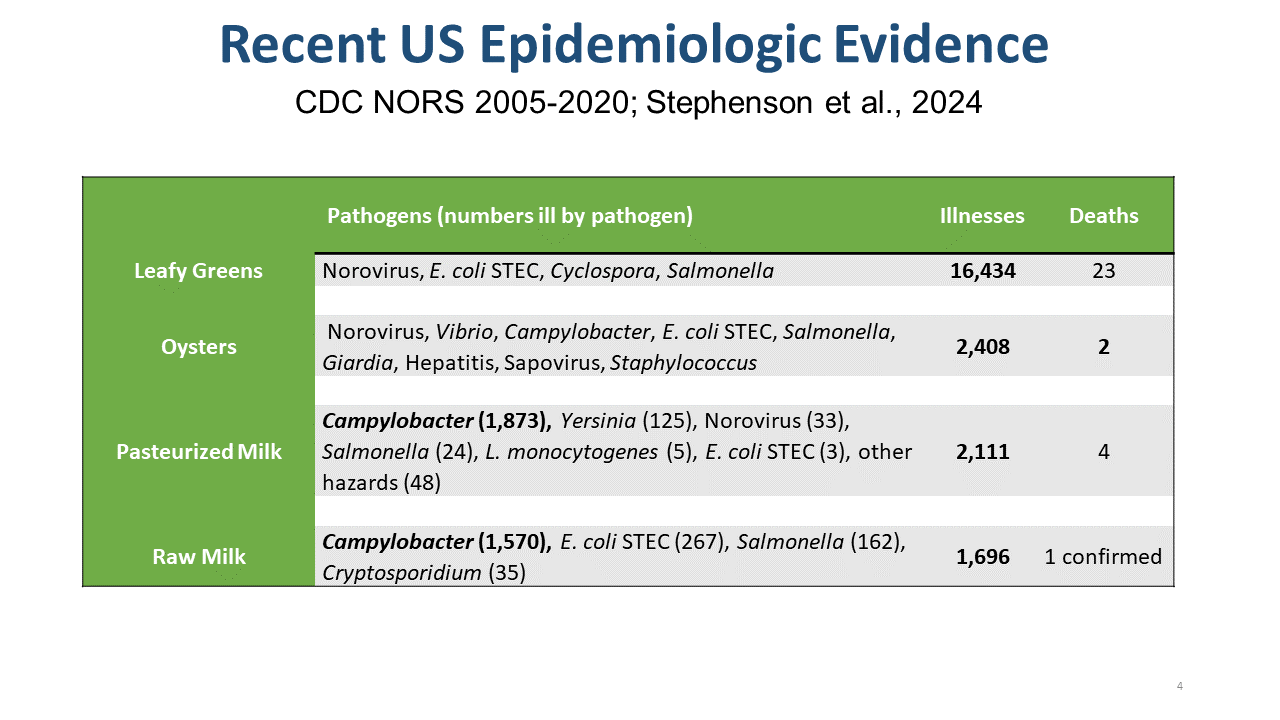
In contrast to the excellent record of saftey for raw milk in NY state and in the US in recent decades, leafy greens and other raw foods pose high burdens of illness and more severe illness, yet are not prohibited from interstate commerce. In fact, no food, including pasteurized milk, is risk-free.
For the period 1971-2023, raw milk illnesses accounted for 0.5% (104/20,278) of foodborne illnesses in NY state, and 0.098% of illnesses from all transmission sources (animal contact, food, person-to-person, water) in NY state.
Note that the burdens of illness from epidemiologic reports on pathogen-food pairs are inputs to the consensus framework for microbial risk assessment as only the first step, Hazard Identification (Marks et al., 1998; Codex Alimentarius Commission, 1999). Further evidence is required (Exposure Assessment, Dose-Response Assessment, Risk Characterization) to estimate risk, of course with attendant uncertainty.
In contrast to the pending case in FL, no stillbirth or miscarriage has been associated with raw milk in recent decades (Sebastianski et al., 2022; Stephenson et al., 2024). However, pasteurized dairy was associated with 12 cases of premature delivery and 8 miscarriages/stillbirths/fetal deaths (Sebastianski et al., 2022), all associated wtih L. monocytogenes.
Please add references to additional evidence, as well as your questions and comments.